An Interview with Alanna Betts, MA, LPC, ATR, PMH-C
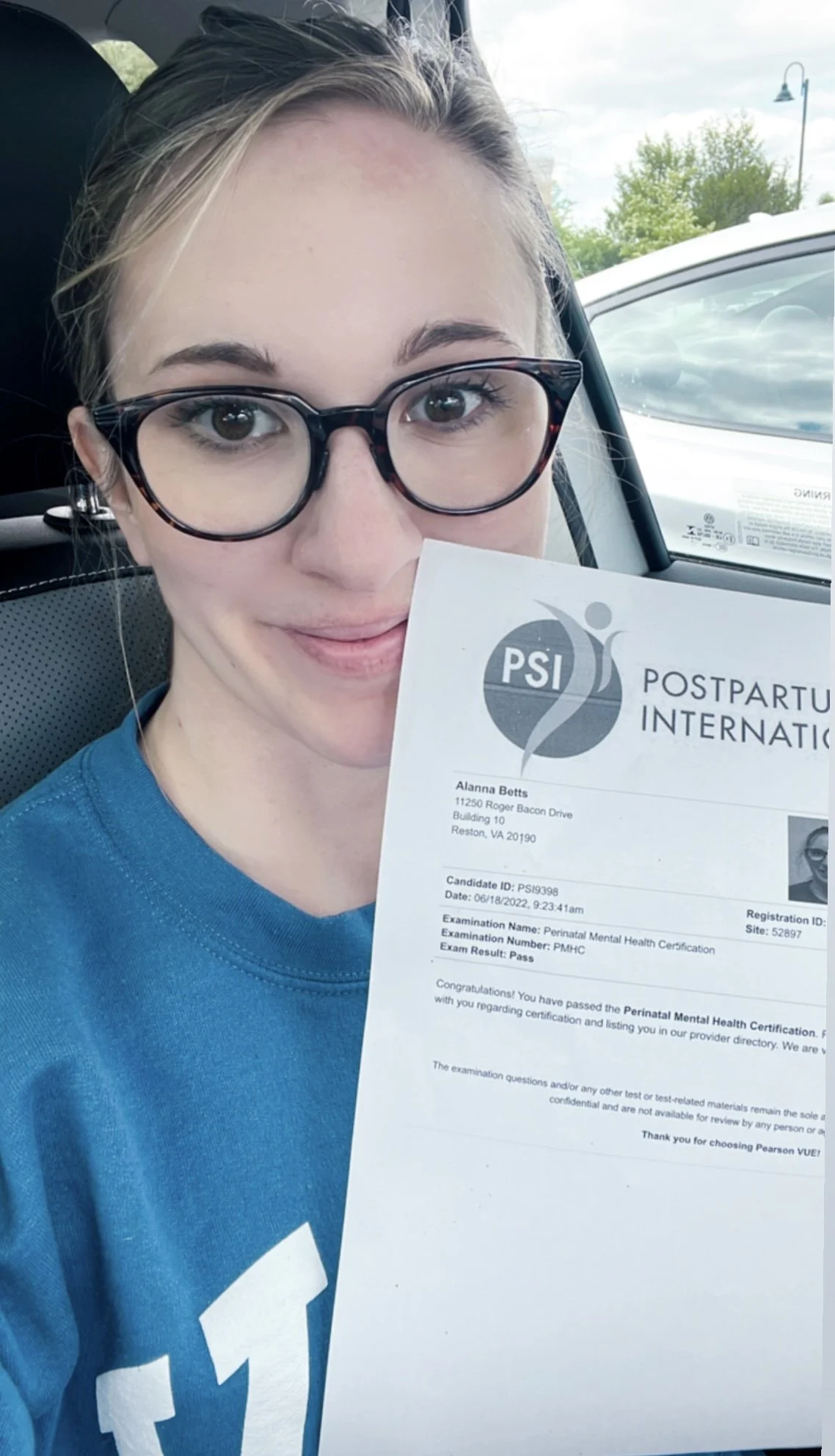
Alanna Betts, MA, LPC, ATR, PMH-C
Finding the right therapist can feel overwhelming. When you are scanning profiles on Psychology Today or reading therapist websites, it is easy to be overwhelmed and unsure. In my over 10 years of practice, I’ve found it so important for my clients to get to know me as person, as well as a professional. I structured this blog as an interview, to share more about me, who I am as a therapist, what guides my work, and how I support clients through healing with creativity, compassion, and evidence-based care.
Can you share a bit about your journey into becoming a therapist?
My journey into becoming a therapist began when I was 16, while receiving treatment for an eating disorder. During that time, I experienced firsthand the profound impact of art therapy. I had always loved making art, but in treatment, art became something more. Art offered a powerful way to process trauma, express emotions that felt difficult to put into words, and begin developing a healthier sense of identity as I moved into recovery.
Years later, while I was an undergraduate student, I survived a traumatic car accident. My professors encouraged me to “make art about it,” and once again, I experienced the healing capacity of the creative process. Through large-scale paintings, ceramic work, and an edition of artist books, I found relief, meaning, and a sense of integration after trauma. Creating allowed my nervous system to settle in ways that talking alone had not.
Although I had already planned to attend graduate school for art therapy and counseling, this experience reignited and deepened my commitment to the field. I went on to complete my graduate training at The George Washington University, whose art therapy program felt like a strong fit for the kind of trauma-focused, clinically rigorous education I was seeking. I am deeply grateful for my training there, particularly for its emphasis on trauma-informed care and the integration of Art Therapy, counseling, and evidence-based care.
You specialize in eating disorders, perinatal mental health, and trauma. What led you to focus on these areas?
In the early years of my career, I focused primarily on developing expertise in the treatment of trauma and eating disorders. While my initial interest was informed by lived experience, it grew and deepened as I worked with clients across inpatient, residential, and PHP/IOP levels of care. Witnessing clients move toward recovery was both humbling and inspiring.
During this time, I completed advanced clinical trainings in trauma and eating disorder treatment, including training through the Embodied Recovery Institute. These experiences reinforced my understanding of how closely trauma, the nervous system, and one’s relationship with the body are intertwined.
While serving as Program Director at a residential eating disorder treatment center, I worked with a woman who had recently given birth and was forced to leave her newborn to receive life-saving care. That experience profoundly shifted my perspective. I became acutely aware of the limitations within traditional treatment models and the deep, often overlooked intersections between eating disorders, trauma, and perinatal mood and anxiety disorders.
In 2020, I completed both the Components of Care and Advanced Perinatal Psychotherapy trainings through Postpartum Support International and began expanding my outpatient work with perinatal clients. In 2022—while pregnant with my first son—I earned my PMH-C (Certified in Perinatal Mental Health) credential. I later completed advanced trainings in birth trauma, infertility, and the intersection of eating disorders and pregnancy.
As my work continued to evolve, I recognized the need for additional tools to support deeper trauma processing. In 2023, I completed my EMDR therapy training, allowing me to help clients move more fully toward healing and integration.
Many of the clients I work with are carrying invisible stories held in their bodies, their past experiences, their births, and their sense of self. My specialties in trauma therapy, eating disorder recovery, and perinatal mental health all center on these intersections of body, identity, and lived experience.
How does your own lived experience inform your work as a therapist?
My recovery from my eating disorder and my own journey into motherhood has deeply shaped how I show up in the therapy room. We all have stories and we all have the potential for healing. My journey provides deeper insights, empathetic connection, and authentic understanding.
While my clinical training guides my work, my personal experiences help me attune more deeply to the emotional complexity many clients carry.
What kinds of clients tend to feel most at home in your practice?
My clients are often thoughtful, resilient, and deeply self-aware. Often they would not describe themselves that way, but I see those features in them during every session.
Clients who often feel most at home in my practice include:
Mothers and mothers-to-be navigating pregnancy or postpartum mood, anxiety, challenges
Individuals healing from birth trauma or reproductive trauma
Women struggling with the pressures of motherhood or the identity shift of being a mom
Adults and teens struggling with Eating Disorders or Body Image concerns
Clients with Eating Disorders who need a therapist comfortable with working outside of the box, supporting their autonomy, and taking a harm reduction approach when needed
Adults who have experienced trauma or complex trauma and struggle to fully leave behind the reminders of their past
Highly sensitive, reflective, or creative individuals
Those seeking depth-oriented, relational therapy rather than quick fixes
Clients who feel disconnected from their bodies
Why did you choose to build a private pay practice?
I’ve worked with insurance companies across multiple levels of care; including inpatient treatment, residential programs, partial hospitalization, and outpatient practice. In many of these settings, I observed how insurance-driven requirements often prioritize cost containment over what is clinically and emotionally best for clients.
I chose to build a private pay therapy practice so I could offer care that is truly client-centered. This model allows me to provide full 60-minute therapy sessions, individualized treatment planning, increased protection of client privacy, and greater flexibility in therapeutic approaches; especially when working with trauma, eating disorders, and perinatal mental health.
One area where this difference is especially meaningful is during the first therapy session. When I was in-network with insurance, I was required to complete a comprehensive diagnostic assessment during the initial appointment. The pressure to gather extensive information quickly often made it difficult to slow down, remain fully trauma-informed, and allow trust to develop at a natural pace. Spreading assessment and story-gathering across multiple sessions helps ensure clients leave therapy feeling supported and regulated, rather than overwhelmed or retraumatized.
The private pay model allows me to practice ethically and relationally, honoring the nervous system, the therapeutic relationship, and each client’s unique healing process—without the constraints often imposed by insurance-driven care.
If someone is reading this and wondering whether to reach out, what would you like to say to them?
You don’t have to do this alone. You don’t have to have everything figured out. Taking the first step doesn’t mean committing to anything long-term; you are just opening the door to the possibility of support.
You deserve care that honors your story, your pace, and your whole self.
Read more about starting therapy.
If you’re considering therapy and want to explore if we are a good fit, I invite you to schedule a complimentary consultation. I offer in-person sessions in Herndon, Virginia and virtual therapy throughout the state of Virginia.